Boulder Independent Medical Evaluations Therapy (BIMET) emphasizes that cultural competency is vital for high-quality, inclusive healthcare. Their training goes beyond knowledge transfer, focusing on attitudes and skills to offer respectful, culturally sensitive services. By integrating Mind Over Matter principles, BIMET boosts resilience, patient satisfaction, and workplace relationships. This approach leads to better diagnoses, tailored therapy plans, and reduced healthcare disparities, particularly for underrepresented communities. Effective training includes interactive workshops, case studies, and role-playing scenarios, ensuring professionals are skilled in unbiased assessment, empathetic care, and mental health advocacy. Measuring success involves skill evaluation, patient feedback, and outcome assessments, with continuous improvement driven by data from sessions, workshops, and surveys.
Healthcare provider cultural competency training is a vital component of modern medical practice, especially in diverse communities like Boulder. This article delves into the necessity of cultural competency in healthcare and explores its significant impact on patient outcomes and provider well-being. We examine designing effective training programs tailored for Boulder Independent Medical Evaluations Therapy (BIMET), as well as assessing success through continuous improvement strategies. By enhancing cultural competence, BIMET can deliver more personalized and effective care to a wide range of patients.
- Understanding Cultural Competency in Healthcare: A Necessary Approach
- The Impact of Training on Patient Outcomes and Provider Well-being
- Designing Effective Training Programs for Boulder Independent Medical Evaluations Therapy
- Measuring Success: Assessment and Continuous Improvement Strategies
Understanding Cultural Competency in Healthcare: A Necessary Approach

In today’s diverse healthcare landscape, understanding cultural competency is no longer an option but a necessity. Boulder Independent Medical Evaluations Therapy recognizes that effective patient care demands providers who can navigate complex cultural differences and create inclusive environments. Cultural competency goes beyond basic knowledge; it involves developing attitudes, skills, and behaviors that enable healthcare providers to deliver respectful, equitable, and culturally sensitive services to patients from various backgrounds.
This approach is crucial for preventing burnout among healthcare professionals. By integrating Mind Over Matter principles into Healthcare Provider Cultural Competency Training, practitioners can enhance their resilience, improve patient satisfaction, and foster healthier relationships within the workplace. Ultimately, a culturally competent healthcare system benefits both providers and patients, ensuring quality care that respects individual differences and promotes overall well-being.
The Impact of Training on Patient Outcomes and Provider Well-being

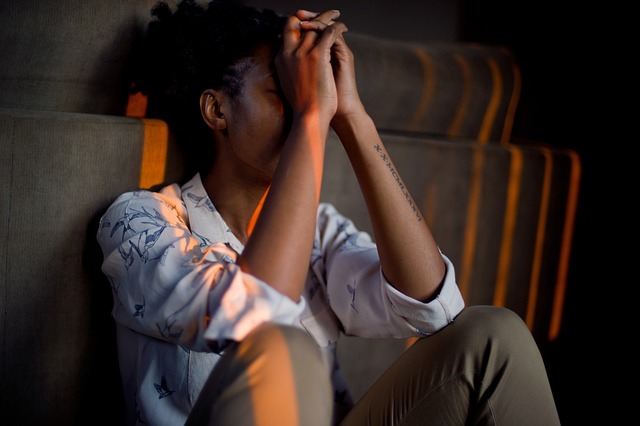
Cultural competency training plays a pivotal role in enhancing patient outcomes and provider well-being. By equipping healthcare professionals with the knowledge and skills to navigate diverse cultural backgrounds, these programs foster better communication and understanding between patients and care providers. This, in turn, leads to improved patient satisfaction, increased adherence to treatment plans, and reduced healthcare disparities. For instance, a study conducted in Boulder, Colorado, revealed that independent medical evaluations (IMEs) incorporating cultural sensitivity guidelines resulted in more accurate diagnoses and tailored therapy plans, particularly for patients from underrepresented communities.
Beyond direct improvements in patient care, training in cultural competency contributes to the mental wellness of healthcare providers. By promoting understanding and empathy towards different cultural perspectives, it reduces stress and burnout related to navigating complex interpersonal dynamics. This positive impact is further amplified when combined with practices such as journaling, exercise guidance, and trauma support services tailored to address the unique challenges faced by professionals working in diverse settings. Incorporating these initiatives ensures that providers not only deliver high-quality care but also maintain their own well-being in the process.
Designing Effective Training Programs for Boulder Independent Medical Evaluations Therapy

Effective training programs for Boulder Independent Medical Evaluations Therapy (BIMET) must be tailored to address the unique cultural nuances of the communities BIMET serves. Incorporating interactive workshops, case studies reflecting diverse patient backgrounds, and role-playing scenarios centered around common challenges in mental health care can significantly enhance learning. This immersive approach allows medical evaluators to develop culturally competent skills, ensuring they provide unbiased, empathetic, and effective care for all individuals, regardless of their background or identity.
Integrating Mental Health Awareness, Crisis Intervention Guidance, and Mental Health Policy Analysis and Advocacy into training curricula equips BIMET professionals with a holistic understanding of the broader systemic issues impacting patient outcomes. By fostering empathy and critical thinking, these programs enable evaluators to not only accurately assess mental health conditions but also advocate for equitable access to care and promote positive policy change within their communities.
Measuring Success: Assessment and Continuous Improvement Strategies

Measuring success in healthcare provider cultural competency training is paramount to ensure meaningful and impactful change. Assessment strategies should go beyond mere knowledge testing to encompass skill evaluation, patient feedback, and outcome measures. Incorporating tools like role-playing scenarios, case studies reflecting diverse patient populations, and post-training follow-ups can provide a comprehensive view of improvement.
Continuous improvement requires a cycle of reflection and action. Regularly collecting and analyzing data from various sources—including Boulder Independent Medical Evaluations Therapy sessions, social skills training workshops, and patient satisfaction surveys—enables trainers to identify areas needing further attention. Integrating this feedback into future training sessions through revised curricula and enhanced activities facilitates the emotional healing processes and promotes better emotional regulation among healthcare providers. Additionally, Social Skills Training components can be refined to meet evolving cultural needs, ensuring that each session builds upon previous learning experiences for optimal results.
Cultural competency training is a game-changer in healthcare, particularly for providers conducting Boulder Independent Medical Evaluations Therapy. By understanding and addressing cultural differences, these training programs enhance patient outcomes, improve provider well-being, and foster better communication. Implementing effective training, as outlined in this article, ensures that healthcare professionals are equipped to navigate complex patient interactions with sensitivity and expertise. Continuous assessment and improvement strategies are vital to maintaining high standards, ensuring a more inclusive and compassionate healthcare environment.